Submitted by Christine Georgiou on Wed, 01/04/2020 - 16:08
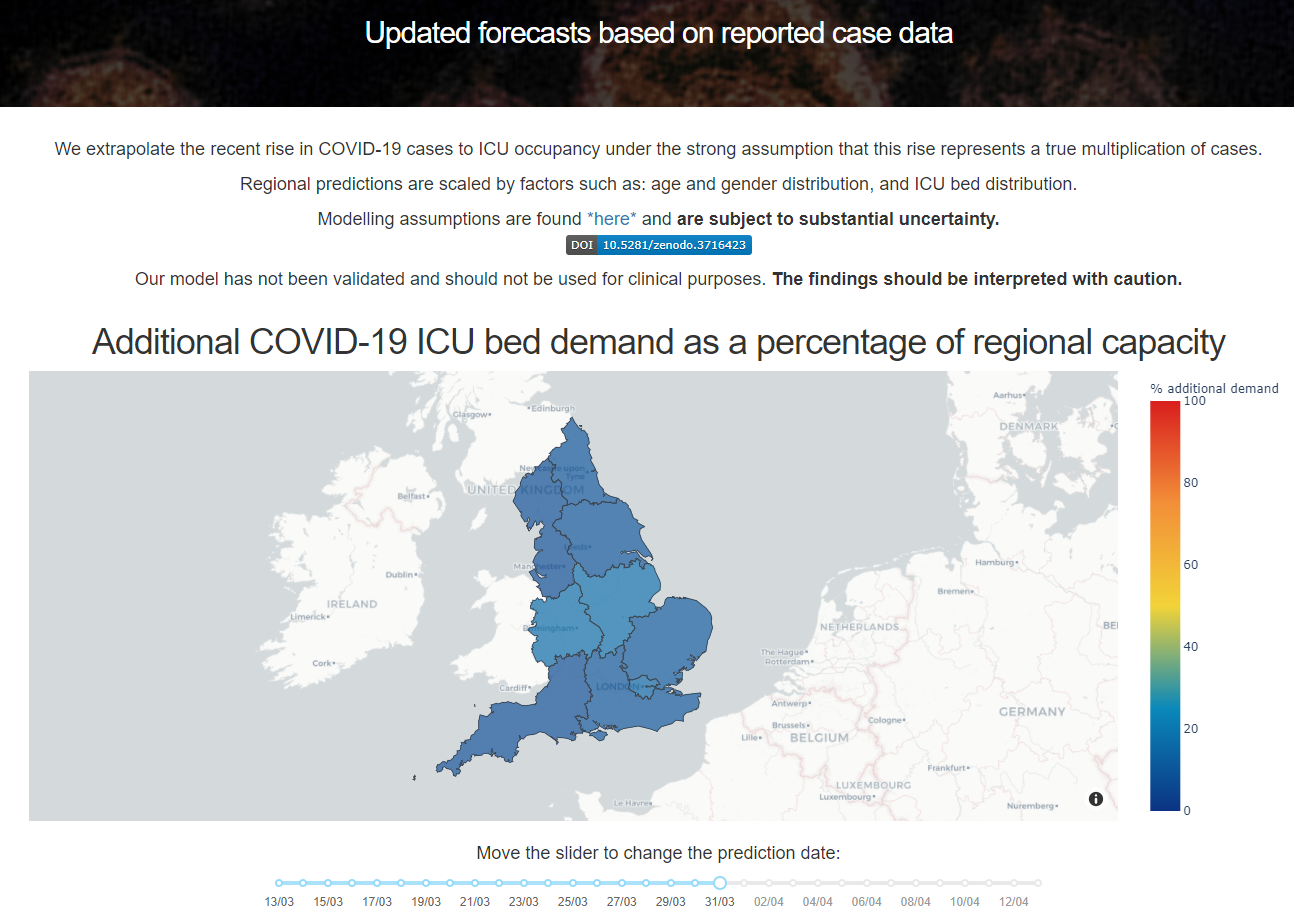
NHS regions in England are using a computer model co-developed by this department to help them predict the surge in demand for intensive care beds caused by the COVID-19 outbreak.
The model was created over eight days of intense collaborative research from 14th to 22nd March and is updated daily. It predicts that if the current exponential growth of COVID-19 infections continues, demand for intensive care beds will increase dramatically over the next two weeks to the point where, without action, they would be overwhelmed.
The real-time model was produced to try and make the earliest possible predictions of intensive care unit (ICU) demand in England. The aim was to give an early warning of when and where capacity would become critical, and give as much advanced notice as possible to help build capacity.
“This is a crucial concern,” explains Dr Ari Ercole, an intensive care consultant at Addenbrooke’s Hospital and one of the research team, “as additional ICU capacity takes time to create both in terms of staffing and equipment.”
The model has been shared with two NHS commissioning regions. After the model was published online, and a preprint of the research paper was circulated because of the urgent implications of the findings, the researchers were contacted by the Midlands commissioning region, and have shared their raw data with them.
“The number of COVID-19 patients so severely ill they need an ICU bed will be equivalent to the entire number of beds for critical care patients in that region.” Jacob Deasy.
 The researchers have also been in consultation with staff from the East of England commissioning region who were seeking information to help them plan future ICU bed numbers.
The researchers have also been in consultation with staff from the East of England commissioning region who were seeking information to help them plan future ICU bed numbers.
The model is being hosted online within this department, with the assumptions that support it being made available alongside it.
It shows that the situation will be particularly acute in London, as might well be expected. What is more surprising, though, is the forecast coming from the model that the Midlands will be equally hard hit.
“We predict that in two weeks’ time, London and the Midlands will have additional demand equivalent to 100% of standard capacity,” says Jacob Deasy, a PhD student in this department who worked on extrapolating the ICU demand from data supplied by Public Health England. “In other words, the number of COVID-19 patients who have become so severely ill they need an ICU bed will be equivalent to the entire number of beds for critical care patients in that region.
“That is because, although London has more beds per capita than anywhere else in the country, the higher incidence rate per capita still takes up the extra capacity. Whereas in the Midlands, they have fewer beds per capita, but a population with a higher average age who are more vulnerable.”
In fact, the researchers suggest, five out of seven commissioning regions in England will have more critically ill COVID-19 patients than can be accommodated with the ICU beds normally available.
Model inspired by decade-old ‘Swine Flu’ study
The model was created by a collaborative research team that spans computer science and intensive care medicine. It was inspired by a previous research carried out by Dr Ercole in 2009 when he and colleagues modelled the impact of that year’s Swine Flu pandemic (H1N1) – which was particularly affecting children – on demand for paediatric intensive care beds.
Early in March, Dr Ercole suggested developing a model to predict ICU demand arising from the coronavirus outbreak and recruited collaborators in this department to help. They include Professor Liò, a member of this department’s Artificial Intelligence group whose research interests include developing Artificial Intelligence and Computational Biology models to understand disease complexity. He has been involved in the modelling and the coding of the host website, as has PhD student Jacob, who was recruited as his PhD research, using healthcare time series, is being jointly supervised by Ari along with Professor Liò. And another of Pietro’s PhD students here, Emma Rocheteau, is also part of the research team that produced this model.
Rapid response more important than perfect assumptions
The deliberate aim was to produce a rapid response, rather than strive for perfect assumptions, because of the urgency of the situation. Subsequently, the initial findings have already been tweaked and adjustments are being made daily. There is also a web tool that allows users to adjust the assumptions for their particular region – such as how long patients in that region are typically staying in an ICU bed, or how long it takes from patients being diagnosed to them needing an ICU bed.
In creating the model, the researchers have assumed exponential growth and considered four key factors: the total number of COVID-19 cases; the number of those patients that will need an ICU bed; the delay (or length of time) from diagnosis to requiring intensive care; and the length of time patients will spend in ICU.
The model will stay online for quite some time to come. “We will continue to sustain the website where it’s hosted,” says Jacob. “And if, at some point, the exponential fit starts to weaken – as we all hope – we will need to tweak the model.’’
“But as a rolling two-week warning system, there is no set end date,” he adds. “Sadly, it is reasonable to assume that there will still be issues around accurately predicting ICU capacity due to COVID-19 in a month’s time.”
Clinicians in Intensive Care Unit photo credit: Calleamanecer (WikiCommons)